Revenue leakage, delayed reimbursements, and administrative bottlenecks are ongoing challenges in healthcare. Manual Revenue Cycle Management (RCM) processes often lead to coding errors, claim denials, and inefficiencies that directly impact financial stability.
AI is addressing these gaps. Research by Medical Billers & Coders reveals that AI-powered RCM can accelerate reimbursements by 20-25%, reduce manual errors by 40%, and enhance revenue forecasting accuracy to over 90%. One notable player in this field is RapidClaims, an AI-driven platform designed to revolutionize medical billing and coding.
This blog explores how AI-driven solutions like RapidClaims streamline RCM, minimize revenue loss, and create a more predictable cash flow for healthcare providers.
What is Revenue Cycle Management (RCM)?
Revenue Cycle Management encompasses the financial processes that healthcare providers use to track patient care episodes from registration and appointment scheduling to the final payment of a balance. The cycle includes processes such as medical coding, billing, claims submission, payment collection, and denial management.
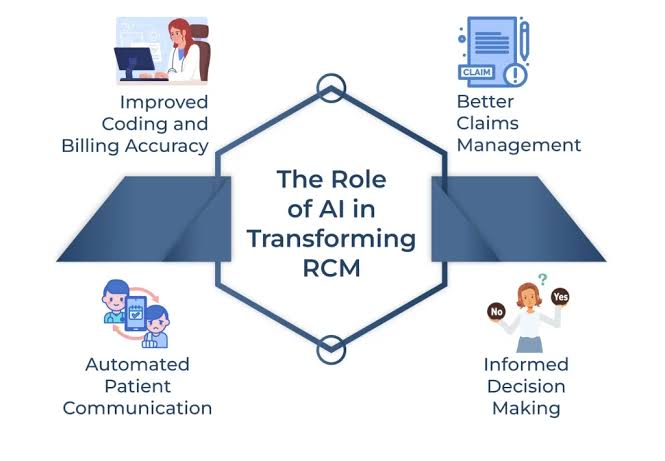
Benefits of AI in Revenue Cycle Management (RCM)
AI is transforming healthcare’s financial workflows by enhancing claims processing, increasing revenue collection, and optimizing revenue cycles. The integration of AI in RCM enables healthcare providers to automate routine tasks, significantly reduce turnaround times for claims, and increase reimbursement rates. Here are some of the key benefits:
1. Enhanced Predictive Analytics
AI-powered RCM solutions offer superior predictive analytics capabilities. Unlike traditional methods that rely on historical data, AI algorithms analyze extensive datasets to forecast trends and identify potential revenue challenges before they escalate. This proactive approach allows healthcare organizations to optimize their financial strategies by anticipating patient payment behaviors and spotting patterns in claim denials.
2. Automation of Billing and Coding
AI automates billing and coding processes, significantly reducing error rates and speeding up the billing cycle. By using Natural Language Processing (NLP) and Machine Learning (ML), AI systems accurately interpret medical documentation, codify diagnoses, and generate claims with minimal errors.
3. Improved Patient Engagement
AI enhances patient engagement through personalized and timely communication. Automated systems remind patients of outstanding bills, offer payment plan options, and efficiently address inquiries. This proactive engagement improves patient satisfaction and financial responsibility, leading to increased revenue collection. AI-driven chatbots and virtual assistants provide patients with easy access to information regarding bills, insurance details, and payment options, fostering trust and improving the overall patient experience.
4. Fraud Detection and Prevention
AI strengthens healthcare organizations’ ability to detect and prevent fraudulent activities. Advanced AI systems monitor financial transactions and claims data to identify anomalies that may go unnoticed in manual audits. This enhances financial integrity within healthcare institutions and strengthens trust in the healthcare system.
5. Efficient Workflow and Resource Utilization
AI streamlines workflows by automating routine tasks, freeing up human resources for more complex and strategic activities. Automating tasks such as data entry, claim processing, and eligibility verification allows RCM professionals to focus on strategic decision-making. This efficient allocation of resources reduces costs and improves productivity.
6. Data-Driven Decision Making
AI transforms the revenue cycle into a data-driven environment. By analyzing vast datasets, AI provides actionable insights into patient information, payment trends, and historical data, enabling healthcare organizations to make informed decisions that optimize revenue and reduce financial risks. Real-time data analytics allow RCM teams to quickly respond to industry changes, regulatory shifts, and changes in reimbursement models, enhancing their adaptability in the dynamic healthcare finance landscape.
Challenges in Traditional Revenue Cycle Management
Traditional RCM processes often involve manual tasks that are time-consuming and prone to errors. Common challenges include:
- Manual Errors: Human errors in data entry and coding can lead to claim denials or delays.
- Inefficient Processes: Manual handling of billing and coding is labor-intensive and slows down the reimbursement cycle.
- Claim Denials: Inaccurate documentation or coding errors can result in denied claims, affecting cash flow.
- Rising Operational Costs: Administrative burdens increase operational costs, diverting resources from patient care.
How RapidClaims Enhance RCM with AI
RapidClaims is an AI-driven medical coding automation platform that transforms medical coding and streamlines Revenue Cycle Management (RCM) processes. By harnessing AI and automation, it boosts coding accuracy, accelerates revenue cycles, and ensures adherence to evolving industry standards. The platform integrates seamlessly with healthcare entities, providing automated coding, workflow optimization, and real-time insights to minimize claim denials and expedite revenue cycles.
Core Features:
RapidClaims offers a comprehensive suite of AI-powered solutions:
- RapidCode: Fully automates medical coding, eliminating manual errors and ensuring precision.
- RapidAssist: Assists human coders with AI-driven suggestions and documentation analysis.
- RapidRisk: Optimizes risk-adjusted coding for improved reimbursements.
These solutions collaborate to automate routine coding tasks, support coders with AI recommendations, and refine risk-adjusted coding for enhanced reimbursement accuracy.
Key Benefits:
- Efficient Automation: RapidClaims automates coding processes or provides AI-assisted recommendations, processing thousands of charts with high accuracy.
- Compliance and Transparency: Ensures adherence to coding guidelines, maintaining a detailed audit trail for every assigned code.
- Informed Decision Making: Identifies coding errors and missing documentation before claim submission, enhancing claim acceptance rates through real-time insights.
- Customization and Security: Tailors coding logic to specific specialties and automates updates based on payer rules. It is HIPAA-compliant, encrypted, and securely hosted.
By integrating these features, RapidClaims significantly reduces claim denials, accelerates revenue cycles, and lowers administrative costs, thereby enhancing the financial efficiency and compliance of healthcare organizations.
RapidClaims stands out from traditional coding solutions by leveraging AI-driven automation to eliminate manual inefficiencies and enhance accuracy. This approach not only improves coding precision but also accelerates the revenue cycle by automating routine tasks, reducing errors, and ensuring compliance with evolving industry standards.
Key Differentiators
- AI-Driven Automation: RapidClaims uses AI to automate medical coding, significantly reducing manual errors and improving accuracy. This automation also helps in identifying up-coding opportunities, enhancing the Clinical Documentation Improvement (CDI) process, and reducing claim denials.
- Seamless Integration: The platform integrates smoothly with Electronic Health Records (EHRs), HL7, FHIR, and billing systems, ensuring a cohesive workflow across different healthcare systems.
- Regulatory Compliance: RapidClaims ensures strict adherence to coding guidelines such as ICD-10, CPT, E&M, and HCC, minimizing the risk of audits and penalties.
- Rapid Implementation: Unlike traditional systems that require extensive setup times, RapidClaims can be implemented within a week, significantly reducing onboarding time and allowing healthcare providers to quickly benefit from its advanced features.
Future of AI in RCM and RapidClaims’ Vision
The future of healthcare financial operations hinges on adopting AI in healthcare revenue cycle management. Predictive analytics powered by AI enables providers to forecast claim outcomes and optimize billing processes. Moreover, AI-driven innovations like automated prior authorizations not only improve operational efficiency but also boost patient satisfaction.
RapidClaims is committed to evolving with AI and machine learning advancements to continue offering cutting-edge solutions that meet the dynamic needs of healthcare providers. The company’s vision includes expanding its AI capabilities to further enhance RCM efficiency, reduce administrative burdens, and improve financial outcomes for healthcare organizations.
Conclusion
The integration of AI into Revenue Cycle Management is more than an operational improvement—it’s a strategic necessity for building a sustainable healthcare system. RapidClaims exemplifies how AI can revolutionize medical billing and coding, leading to enhanced efficiency, reduced errors, and improved financial performance. As the healthcare industry continues to evolve, embracing AI-driven solutions like RapidClaims will be crucial for organizations aiming to optimize their RCM processes and focus more on delivering quality patient care.
For healthcare providers seeking to enhance their RCM efficiency, exploring AI-driven solutions like RapidClaims is a proactive step toward achieving financial sustainability and operational excellence